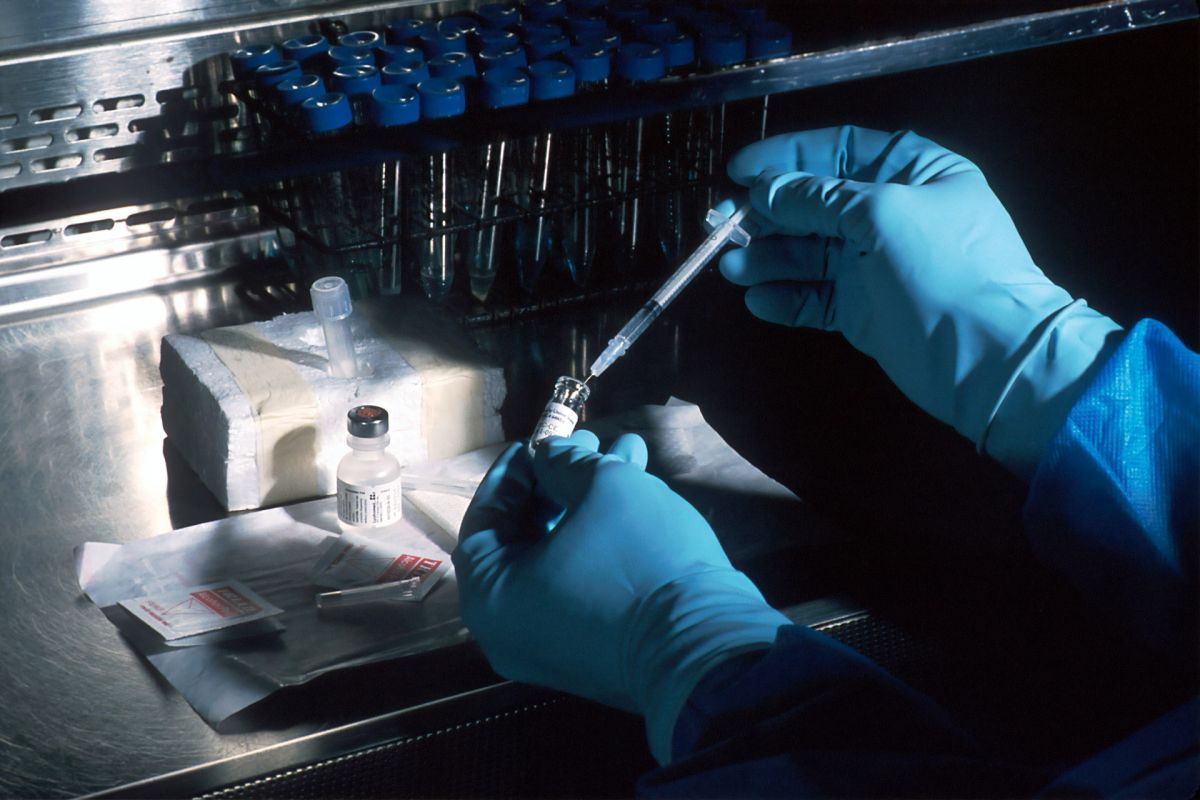
The race to develop a vaccine for COVID-19 is on, and with it comes a barrage of ethical concerns. So far the ethical considerations have focused on clinical trials, like the speed at which researchers are moving to human subjects, but there is little discussion on the role of ethics in the post-market regulation and surveillance of an eventual COVID-19 vaccine.
Historically, the primary evidence of a drug or vaccines efficacy and effectiveness were based on the data from clinical trials, but over the last 2 decades there has been a growing recognition that government bodies responsible for ensuring the safety and effectiveness of pharmaceuticals face serious challenges when protecting the public from harm once these products are used by people in the uncontrolled, real-world context. The reality is when drugs and vaccines first enter the market there are many things we don’t know. Historically drug regulation has relied primarily on the evidence provided by clinical trials, but even the most honestly conducted clinical trials face three primary limitations. First, clinical trials are conducted under controlled conditions that do not necessarily reflect how a drug will be used in real life, and miss extenuating environmental influences. Second, clinical trials tend to detect common and frequently occurring adverse drug events, but miss important ones that take longer to occur. Third, clinical trials lack diversity with most participants being white males between 20-30. In light of these limitations, there has been a gradual move by most regulatory bodies towards a lifecycle approach to drug regulation. A lifecycle approach increases focus on the surveillance and evidence gathering of how drugs and vaccines behave once they enter the market.
Many will argue that in the case of COVID-19, time for cautious post-market surveillance is not a luxury we have; but we cannot ignore the inherent risks of brand new drugs/vaccines. For the COVID-19 vaccine, the consequences of rushed distribution will be blatantly apparent given the mass distribution that will occur immediately after successful clinical trials are completed. The Serum Institute in India for instance, one of the world’s largest vaccine producers, is mass-manufacturing a vaccine developed by the Jenner Institute at Oxford University that has yet to be proven efficacious. They intend to have 40-50million doses ready by September. By the time any adverse effects are discovered that were missed in clinical trials they will have impacted astronomically more people than the average drug would. This wouldn’t only impact the health of those suffering from the adverse effects; it would also strengthen anti-science movements like the anti-vaxxers.
That being said, the mass distribution of the vaccine is, at this point, inevitable. Therefore, we must consider how to ensure the safety of the population once the vaccine has entered the market. In order to ethically distribute the COVID-19 vaccine there are a number of considerations we must make. First, it is the moral obligation of physicians, pharmacists and regulators to ensure that people are not harmed due to a lack of safety or effectiveness. To do that, decisions must be made based on the highest quality of evidence possible; regulators should be prepared to review their decisions based on any new evidence that comes to light, even if it means withdrawing the vaccine from the market; regulators and health care professionals have a duty to warn people of any safety/effectiveness issues that exist with the vaccine; and regulatory bodies must conduct post-market surveillance to monitor the safety/effectiveness of the vaccine in order to collect data to support the aforementioned points.
Second, the rationale for regulatory decisions, as well as the decisions themselves, ought to be transparent and communicated with the public. Risk communication around safety issues should be made accessible and understandable to the public so that they can make informed decisions. Third, the public must accept the risk-benefit profile of the vaccine. In a pandemic like this, the public will likely be more accepting of vaccines with less evidence of safety and efficacy, but that strengthens the case of more stringent monitoring.
In all likelihood, the benefit of the vaccine will outweigh the risks as side effects are typically quite rare; especially given the devastation COVID-19 is causing everywhere from nursing homes to prenatal units. However, in order to confirm that, and maintain public trust, regulators and health care professionals must keep in mind the ethics of post-market surveillance once the vaccine has entered the market.